Diabetes is a long-term condition that affects millions of people around the world. Understanding diabetes symptoms, causes, and treatments is important. This knowledge helps you manage your health better.
You may have heard about diabetes, but do you know how it impacts your body and what signs to look out for? You’ll discover what diabetes is and how it affects your blood sugar levels. We will look at the common symptoms of diabetes. These include feeling extremely hungry, being incredibly thirsty, and having wounds that heal sluggishly. We will also discuss the factors that increase your risk.
You’ll also learn about the diagnostic process, various treatment options like insulin therapy, and strategies to manage diabetes effectively. You will see how easy it is to find a doctor online with the Dr Do Good Platform for managing diabetes. If you are concerned about prediabetes, type 1 diabetes, or type 2 diabetes, this guide is for you. This resource is also for anyone who wants to stay informed about diabetes.
What is Diabetes?
Definition
Diabetes is a chronic metabolic condition characterized by elevated blood glucose levels. It occurs when your body either doesn’t produce enough insulin or can’t use insulin effectively. Insulin, a hormone produced by the pancreas, plays a crucial role in regulating blood sugar levels. When you have diabetes, your body struggles to maintain normal blood glucose levels, which can lead to various health complications over time.
Types of Diabetes
There are several types of diabetes, each with its own unique characteristics:
- Type 1 Diabetes: This is an autoimmune condition where your immune system mistakenly attacks and destroys the insulin-producing beta cells in your pancreas. As a result, your body produces little or no insulin. Type 1 diabetes often develops in children and young adults, but it can occur at any age.
- Type 2 Diabetes: This is the most common form of diabetes, accounting for about 90% of all cases. In type 2 diabetes, your body becomes resistant to insulin or doesn’t produce enough insulin to maintain normal blood glucose levels. It typically develops in adults, but it’s increasingly being diagnosed in younger people due to sedentary lifestyles and obesity.
- Gestational Diabetes: This type occurs during pregnancy when hormonal changes cause insulin resistance. It usually resolves after childbirth, but women who experience gestational diabetes have an increased risk of developing type 2 diabetes later in life. Read about how diabetes affect women’s health.
- Prediabetes: This condition is characterized by blood glucose levels that are higher than normal but not high enough to be diagnosed as type 2 diabetes. It’s often a precursor to type 2 diabetes.
How Insulin Works For Diabetes

To understand diabetes, it’s essential to know how insulin functions in your body. Insulin is a hormone that acts as a key, allowing glucose to enter your cells and provide energy. Here’s how it works:
- After you eat, your digestive system breaks down carbohydrates into glucose, which enters your bloodstream.
- Your pancreas detects the rise in blood glucose levels and releases insulin.
- Insulin helps your cells absorb glucose from the bloodstream, lowering your blood sugar levels.
- Excess glucose is stored in your liver and muscles as glycogen for later use.
In diabetes, this process is disrupted. If you have type 1 diabetes, your body doesn’t produce insulin, so glucose can’t enter your cells. In type 2 diabetes, your cells become resistant to insulin, making it difficult for glucose to enter. As a result, glucose builds up in your bloodstream, leading to high blood sugar levels.
Understanding the different types of diabetes and how insulin works is crucial for managing the condition effectively. By maintaining healthy blood glucose levels through proper diet, exercise, and medication (if necessary), you can reduce the risk of complications and lead a fulfilling life with diabetes.
Signs and Symptoms of Diabetes
Recognizing the symptoms of diabetes is crucial for early detection and management of the condition. While some symptoms are common to all types of diabetes, others are specific to type 1 or type 2 diabetes. Let’s explore these symptoms in detail.
General Symptoms
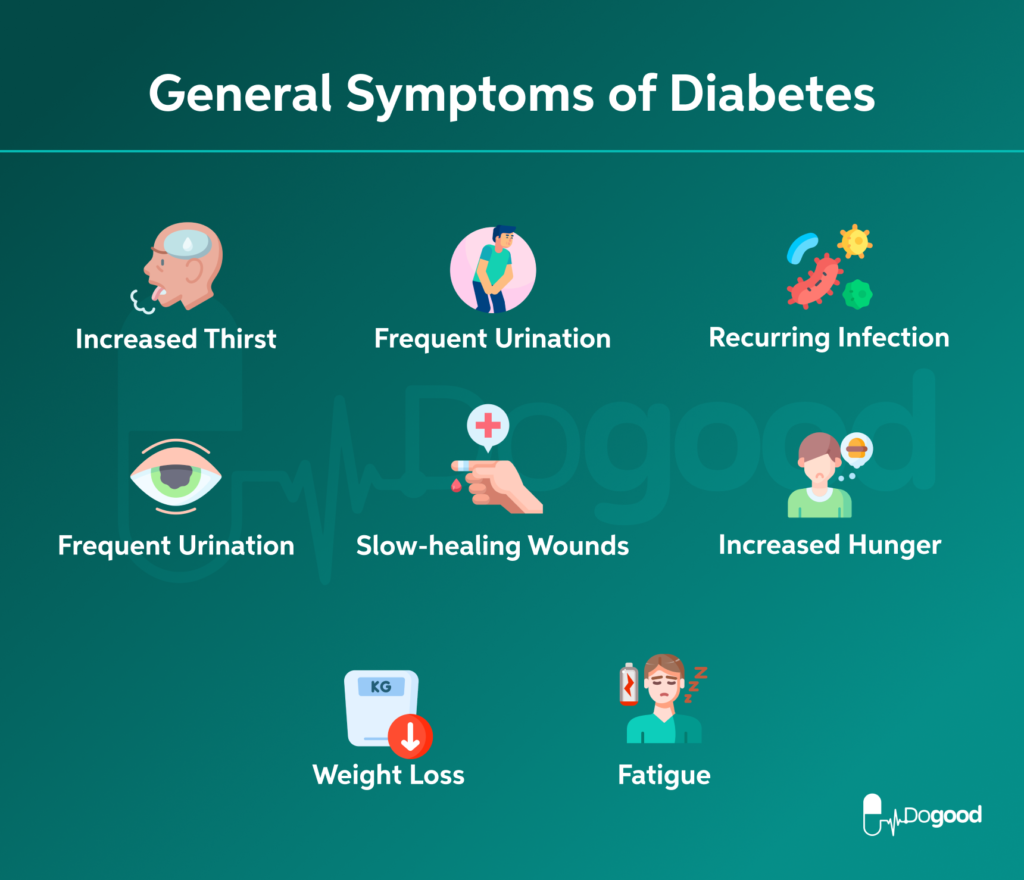
The most common symptoms of diabetes include:
- Increased thirst: You may find yourself feeling excessively thirsty, even after drinking plenty of fluids.
- Frequent urination: You might notice that you’re going to the bathroom more often, especially at night.
- Fatigue: Feeling unusually tired or worn out is a common sign of diabetes.
- Blurred vision: High blood sugar levels can cause changes in the shape of your eye’s lens, leading to blurry vision.
- Slow-healing wounds: Cuts and sores may take longer to heal than usual.
- Unexplained weight loss: Despite eating normally or even more than usual, you might experience unintentional weight loss.
- Increased hunger: You may feel hungry more often, even shortly after eating.
- Recurring infections: You might experience frequent yeast infections or urinary tract infections.
Symptoms Specific to Type 1 Diabetes
Type 1 diabetes symptoms often develop quickly, typically over a few weeks or months. The most common signs include:
- Rapid onset of symptoms: The 4Ts of type 1 diabetes (Toilet, Thirsty, Tired, Thinner) often appear suddenly and progress rapidly.
- Extreme thirst and frequent urination: These symptoms are usually more severe in type 1 diabetes.
- Sudden weight loss: Despite increased hunger, you may lose weight rapidly.
- Diabetic ketoacidosis (DKA): This life-threatening complication can occur if type 1 diabetes is left untreated. Symptoms of DKA include:
- Fruity-smelling breath
- Nausea and vomiting
- Abdominal pain
- Rapid breathing
- Confusion or drowsiness
If you experience these symptoms, seek immediate medical attention, as DKA requires urgent treatment.
Symptoms Specific to Type 2 Diabetes
Type 2 diabetes symptoms often develop more slowly and can be subtle. Many people with type 2 diabetes may not notice any symptoms for years. Some specific signs to watch for include:
- Gradual onset of symptoms: Unlike type 1, type 2 diabetes symptoms typically develop slowly over time.
- Darkened skin patches: You might notice dark, velvety patches of skin in body folds and creases, particularly around the neck and armpits. This condition is called acanthosis nigricans and can be a sign of insulin resistance.
- Numbness or tingling: You may experience tingling or numbness in your hands or feet due to nerve damage caused by prolonged high blood sugar levels.
- Frequent infections: Recurring skin, gum, or bladder infections can be a sign of type 2 diabetes.
- Slow-healing wounds: Cuts and sores may take longer to heal, especially on the feet.
It’s important to note that some people with type 2 diabetes may not experience any symptoms at all. In fact, up to 6 out of 10 people have no symptoms when they’re diagnosed with type 2 diabetes. This is why regular check-ups and blood sugar screenings are crucial, especially if you have risk factors for diabetes.
If you notice any of these symptoms, it’s essential to consult your healthcare provider promptly. Early diagnosis and treatment can help prevent complications and improve your overall health and quality of life. Remember, diabetes is a manageable condition, and with proper care and lifestyle changes, you can lead a healthy, fulfilling life.
Causes and Risk Factors For Diabetes
Causes of Type 1 Diabetes
Type 1 diabetes occurs when your immune system attacks and destroys the insulin-producing beta cells in your pancreas. Scientists believe that both genetic and environmental factors play a role in triggering this autoimmune response. While the exact cause remains unknown, research suggests that certain viruses or environmental toxins may trigger the disease in individuals with a genetic predisposition.
The risk of developing Type 1 diabetes varies depending on family history. If you have no family history, your risk is approximately 0.4%. However, if your biological mother has Type 1 diabetes, your risk increases to 1% to 4%, and if your biological father has it, your risk is 3% to 8%. When both biological parents have Type 1 diabetes, the risk can be as high as 30%.
Causes of Type 2 Diabetes
Type 2 diabetes, the most common form of diabetes, results from a combination of factors. Unlike Type 1 diabetes, where the body doesn’t produce insulin, in Type 2 diabetes, your body either doesn’t make enough insulin or can’t use it effectively. This condition, known as insulin resistance, leads to elevated blood glucose levels.
Several factors contribute to the development of Type 2 diabetes:
- Insulin Resistance: This occurs when cells in your muscles, fat, and liver don’t respond well to insulin, making it difficult for glucose to enter cells.
- Genetics: Type 2 diabetes has a strong genetic component, with the disease tending to run in families.
- Lifestyle Factors: Obesity, lack of physical activity, and an unhealthy diet high in simple carbohydrates and fats can increase your risk of developing Type 2 diabetes.
- Age: The risk of Type 2 diabetes increases significantly around age 45 and rises considerably after age 65.
Risk Factors For Diabetes

Several risk factors increase your chances of developing diabetes, particularly Type 2 diabetes:
- Weight: Being overweight or obese is a significant risk factor. Extra weight, especially around the abdomen, can lead to insulin resistance.
- Physical Inactivity: A sedentary lifestyle increases your risk of diabetes. Regular physical activity helps lower insulin resistance and improves glucose utilization.
- Family History: Having a parent or sibling with diabetes increases your risk.
- Age: The risk of Type 2 diabetes increases with age, especially after 35.
- Prediabetes: This condition, characterized by higher-than-normal blood sugar levels, often progresses to Type 2 diabetes if left untreated.
- Gestational Diabetes: Women who had gestational diabetes during pregnancy have an increased risk of developing Type 2 diabetes later in life.
- Polycystic Ovary Syndrome (PCOS): This condition is associated with insulin resistance and an increased risk of Type 2 diabetes.
- Certain Medications: Some medications, such as glucocorticoids and certain antipsychotic drugs, can increase the risk of diabetes.
Understanding these causes and risk factors is crucial for early detection and prevention of diabetes. By maintaining a healthy weight, staying physically active, and managing other risk factors, you can significantly reduce your risk of developing Type 2 diabetes.
Find out your risk of developing diabetes with our free prediabetes test.
Diabetes Diagnosis and Treatment
Diagnosing diabetes involves various blood glucose tests that help determine if your blood sugar levels are higher than the healthy range. These tests are crucial for early detection and management of diabetes.
Blood Glucose Tests
Several blood glucose tests are used to diagnose diabetes:
- Fasting Blood Sugar Test: This test measures your blood glucose level after you’ve fasted for at least 8 hours. A fasting blood sugar level less than 100 mg/dL is considered normal. If your result is between 100 to 125 mg/dL, you have prediabetes. A level of 126 mg/dL or higher on two separate tests indicates diabetes.
- Random Blood Sugar Test: This test can be done at any time, regardless of when you last ate. A blood sugar level of 200 mg/dL or higher suggests diabetes.
- Oral Glucose Tolerance Test (OGTT): For this test, you fast overnight and then drink a sugary liquid. Your blood sugar levels are tested regularly for the next two hours. A reading of more than 200 mg/dL after two hours means you have diabetes. A result between 140 and 199 mg/dL indicates prediabetes.
A1C Test
The A1C test, also known as the glycated hemoglobin test, is a common blood test used to diagnose type 1 and type 2 diabetes. It measures your average blood sugar level over the past two to three months by determining the percentage of blood sugar attached to hemoglobin, the oxygen-carrying protein in red blood cells.
An A1C level of 6.5% or higher on two separate tests indicates diabetes. A result between 5.7% and 6.4% suggests prediabetes. Below 5.7% is considered normal.
The A1C test is particularly useful because:
- It doesn’t require fasting.
- It shows your average blood sugar level over time, rather than just at a single point.
- It’s used to monitor how well your diabetes treatment plan is working if you’ve already been diagnosed.
Your doctor may recommend getting an A1C test twice a year if you don’t use insulin and your blood sugar level is consistently within your target range. If you take insulin or have trouble keeping your blood sugar level within your target range, you might need the test four times a year.
Gestational Diabetes Screening
If you’re pregnant, your doctor will likely test you for gestational diabetes between 24 and 28 weeks of pregnancy. This is because insulin resistance can increase during pregnancy, leading to higher glucose intolerance and the development of gestational diabetes in some pregnant individuals.
The most common screening method is a two-step approach:
- Glucose Challenge Test: You’ll drink a syrupy glucose solution. One hour later, you’ll have a blood test to measure your blood sugar level. A result of 140 mg/dL or higher indicates the need for further testing.
- Follow-up Glucose Tolerance Test: If the glucose challenge test shows high blood sugar levels, you’ll undergo a three-hour glucose tolerance test to confirm the diagnosis.
It’s important to note that gestational diabetes usually goes away after pregnancy. However, it increases your risk of developing type 2 diabetes later in life, so your doctor will likely recommend regular diabetes screening after your baby is born.
Remember, early diagnosis of diabetes is crucial for effective management and prevention of complications. If you experience symptoms of diabetes such as excessive thirst, frequent urination, or unexplained weight loss, don’t hesitate to consult your healthcare provider for appropriate testing.
Got a question about Gestational Diabetes? Get Answers from Trusted Medical Professionals for Free.
Treatment Options for Diabetes
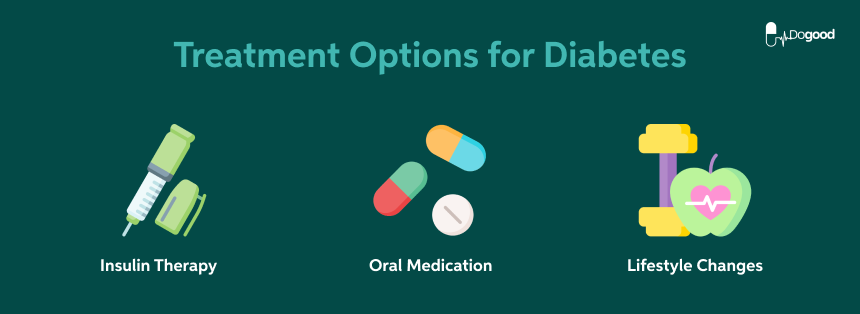
Managing diabetes involves a comprehensive approach that includes lifestyle changes, medications, and regular monitoring of blood glucose levels. The goal is to keep your blood sugar within a healthy range to prevent complications and improve your overall quality of life.
Insulin Therapy
For people with type 1 diabetes and some with type 2 diabetes, insulin therapy is a crucial part of treatment. Insulin helps your body use glucose for energy and regulates blood sugar levels. There are several types of insulin available, each with different onset times, peak effects, and durations:
- Rapid-acting insulin: Starts working within 15 minutes, peaks in 1 hour, and lasts for 2 to 4 hours.
- Short-acting insulin: Reaches the bloodstream in 30 minutes, peaks within 2 to 3 hours, and lasts 3 to 6 hours.
- Intermediate-acting insulin: Begins working in 2 to 4 hours, peaks in 4 to 12 hours, and lasts 12 to 18 hours.
- Long-acting insulin: Starts to work a few hours after injection and works for about 24 hours or longer.
Your healthcare provider will work with you to determine the best insulin regimen based on your individual needs, lifestyle, and blood glucose patterns.
Oral Medications
For many people with type 2 diabetes, oral medications play a significant role in managing blood glucose levels. Some common classes of oral diabetes medications include:
- Metformin: Often considered the first-line treatment for type 2 diabetes, metformin helps lower blood glucose levels by decreasing the amount of glucose produced by the liver.
- Sulfonylureas: These medications stimulate the pancreas to release more insulin, helping to lower blood sugar levels.
- DPP-4 inhibitors: These drugs help improve A1C (a measure of average blood glucose levels over two to three months) without causing hypoglycemia (low blood sugar).
- SGLT2 inhibitors: These medications work in the kidney to increase glucose excretion in the urine, leading to lower blood sugar levels.
- Thiazolidinediones: These drugs help insulin work better in the muscle and fat tissues and reduce glucose production in the liver.
Your healthcare provider may prescribe a combination of these medications to achieve optimal blood glucose control.
Lifestyle Changes
In addition to medication, making lifestyle changes is crucial for managing diabetes effectively. Some key lifestyle modifications include:
- Healthy eating: Follow a balanced diet that includes a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. Carbohydrate counting and the plate method are two common approaches to meal planning for people with diabetes.
- Regular physical activity: Aim for at least 150 minutes of moderate-intensity aerobic activity per week. Exercise helps your body use insulin more effectively and can lower blood sugar levels.
- Weight management: If you’re overweight, losing even a small amount of weight can have a significant impact on your blood sugar control. People who are overweight and lose as little as 7% of their body weight can decrease their risk of diabetes by more than 50%.
- Stress management: Find ways to manage stress through relaxation techniques, hobbies, or activities that help you unwind.
- Quitting smoking: If you smoke, quitting can help reduce your risk of diabetes-related complications.
- Limiting alcohol consumption: If you choose to drink, do so in moderation and be aware of how alcohol affects your blood sugar levels.
Remember, the treatment plan for diabetes is highly individualized. Your healthcare provider will work with you to create a personalized approach that takes into account your specific needs, preferences, and health status. Regular check-ups and monitoring of your blood glucose levels are essential to ensure your treatment plan remains effective over time.
Read about:
Conclusion
Understanding diabetes and its impact on your health is crucial to managing this chronic condition effectively. By recognizing the symptoms, understanding the causes and risk factors, and knowing the various treatment options available, you can take control of your health and lead a fulfilling life with diabetes. Regular check-ups, blood sugar monitoring, and lifestyle changes play a key role in keeping your blood glucose levels in check and preventing complications.
Remember, you’re not alone in this journey. Healthcare professionals, support groups, and educational resources are available to help you navigate life with diabetes. To gain more insights and support, consider joining the lifewithdiabetes program. With the right knowledge, tools, and support system, you can thrive despite diabetes and enjoy a healthy, active lifestyle.
FAQs
What are the symptoms, causes, and treatments for diabetes?
The primary cause of diabetes remains largely unknown, but it generally involves elevated blood sugar levels due to insufficient insulin production by the pancreas. Both Type 1 and Type 2 diabetes might stem from genetic and environmental factors.
What is a significant symptom of diabetes?
Many individuals with diabetes commonly experience increased thirst, frequent urination, fatigue, and weight loss. For a more detailed understanding of diabetes symptoms and their origins, consider watching educational videos on the topic.
How are diabetes symptoms managed?
While Type 2 diabetes cannot be cured, its symptoms can be managed through weight loss, a healthy diet, and regular exercise. If these measures are insufficient, diabetes medications or insulin therapy may be necessary.
What causes diabetes and what are the treatment options available?
Diabetes treatment typically involves insulin or other medications. Healthy lifestyle choices such as a balanced diet, regular physical activity, adequate sleep, and stress management are crucial. There are also other treatment options available to help manage this condition.

