Peptic Ulcer Disease (PUD) is a common digestive condition that causes painful sores in the lining of the stomach or the upper part of the small intestine (duodenum). These ulcers can lead to symptoms such as burning stomach pain, bloating, nausea, and in severe cases, internal bleeding.
The good news is that peptic ulcers are treatable. With the right medical therapy, lifestyle changes, and preventive measures, you can heal ulcers and prevent complications. In this guide we will walk you through the best treatment options and how to manage PUD effectively.
Understanding Peptic Ulcer Disease
Your stomach produces acid to help digest food, but this acid is so strong that it could damage the stomach lining. To protect itself, the stomach has a special mucus layer that acts like a shield.
Peptic ulcer disease happens when something weakens this shield, allowing acid to burn and create open sores (ulcers) in the stomach or the first part of the small intestine (duodenum).
The two most common reasons for this are:
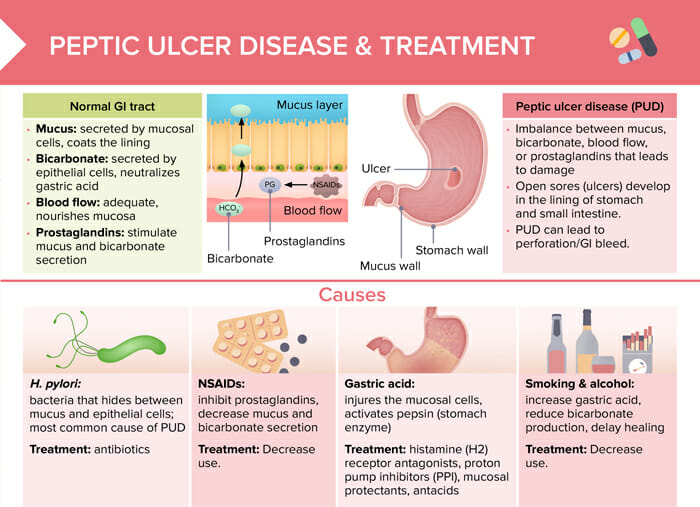
- Frequent use of NSAIDs (painkillers like ibuprofen or aspirin) – These medications reduce the stomach’s ability to produce protective mucus, leaving the lining exposed to acid.
- H. pylori infection – This is a type of bacteria that can survive in the stomach’s harsh environment. It damages the protective mucus layer, making the stomach lining more vulnerable to acid.
Other factors like stress, spicy foods, and smoking can make symptoms worse but don’t directly cause ulcers.
When the acid erodes the stomach lining, it can lead to epigastric pain (which can feel like chest pain), bleeding, and in severe cases, perforation (a hole in the stomach).
Types of Peptic Ulcers
Peptic ulcers are open sores that develop in the lining of the stomach or the upper part of the small intestine due to excessive acid exposure. They are classified based on their location:
1. Gastric Ulcers
- These ulcers form in the lining of the stomach.
- Symptoms often worsen after eating because food triggers acid production, irritating the ulcer.
- More common in older adults
2. Duodenal Ulcers
- These ulcers develop in the first part of the small intestine (duodenum).
- Symptoms tend to improve after eating but worsen a few hours later or at night when the stomach is empty.
- More common in younger adults.
3. Esophageal Ulcers
- These ulcers occur in the esophagus due to acid reflux or chronic irritation from medications or alcohol.
- Symptoms include pain while swallowing, heartburn, and chest pain.
4. Stress Ulcers
- These ulcers develop due to severe stress, such as critical illness, trauma, or major surgery.
- Often found in hospitalized patients, especially those in intensive care.
5. Refractory Ulcers
- These are ulcers that do not heal despite treatment.
- Causes include continued H. pylori infection, excessive NSAID use, or underlying conditions like Zollinger-Ellison syndrome (a rare disorder causing excessive acid production).
Understanding the type of ulcer helps in choosing the right treatment plan for faster healing and symptom relief.
How to Treat Peptic Ulcer Disease
1. Medical Treatments for Peptic Ulcers
The primary goal of treating PUD is to heal the ulcer, relieve symptoms, and prevent complications.
a) Treating H. pylori Infection
If an H. pylori infection is responsible for your ulcer, your doctor will prescribe a combination of antibiotics to eliminate the bacteria.
- Triple Therapy (Standard Treatment)
- Proton Pump Inhibitor (PPI) (e.g., omeprazole, lansoprazole, pantoprazole) – Reduces stomach acid.
- Two Antibiotics (e.g., clarithromycin + amoxicillin or metronidazole) – Kills H. pylori.
- Duration: Typically 10-14 days.
- Quadruple Therapy (For Antibiotic-Resistant Cases)
- PPI + Bismuth subsalicylate (Pepto-Bismol) + Metronidazole + Tetracycline.
- Used when standard therapy fails.
After treatment, a follow-up test (such as a stool antigen test or breath test) is needed to confirm that H. pylori has been eradicated. This is why it’s important that your treatment is directed by a doctor.
b) Medications to Reduce Stomach Acid
Even if H. pylori is not present, reducing stomach acid is essential for ulcer healing. The following medications are commonly prescribed:
- Proton Pump Inhibitors (PPIs) – These are the most effective acid-suppressing drugs, allowing the ulcer to heal faster. Common PPIs include:
- Omeprazole (Prilosec)
- Esomeprazole (Nexium)
- Lansoprazole (Prevacid)
- Pantoprazole (Protonix)
- H2-Receptor Blockers – These drugs also reduce stomach acid but are slightly less effective than PPIs. Examples include:
- Ranitidine (Zantac)
- Famotidine (Pepcid)
- Cimetidine (Tagamet)
- Antacids – These provide quick relief by neutralizing stomach acid but don’t promote ulcer healing. Common antacids include:
- Calcium carbonate (Tums)
- Magnesium hydroxide (Milk of Magnesia)
- Aluminum hydroxide (Maalox)
- Protective Agents (Mucosal Protectants) – These coat the stomach lining, acting as a barrier against acid. Examples include:
- Sucralfate (Carafate) – Forms a protective layer over the ulcer.
- Bismuth subsalicylate (Pepto-Bismol) – Has antibacterial properties against H. pylori.
c) Discontinuing NSAIDs
If NSAIDs caused your ulcer, stopping or reducing their use is crucial. If you need pain relief, your doctor may recommend:
- Switching to acetaminophen (Tylenol) instead of NSAIDs.
- Using low-dose NSAIDs with a PPI for stomach protection.
However be aware that these also carry their risks. You should let your doctor explore the cause of your pain so the source of it can be treated and you can avoid being reliant on painkillers.
2. Lifestyle and Dietary Changes
In addition to medication, making the right lifestyle choices can speed up healing and prevent future ulcers.
a) Eat a Stomach-Friendly Diet
While diet alone doesn’t cause ulcers, certain foods can worsen symptoms. Here’s what you can eat and try to avoid:
- Foods That Help Heal Ulcers
- High-fiber foods (oats, apples, carrots)
- Probiotic-rich foods (yogurt, kefir)
- Lean proteins (chicken, fish)
- Healthy fats (olive oil, avocado, nuts)
- Foods to Avoid
- Spicy foods (may worsen irritation)
- Acidic foods (tomatoes, citrus fruits)
- Fried and fatty foods
- Caffeinated and carbonated drinks
- Alcohol
b) Reduce Stress Levels
Stress doesn’t directly cause ulcers but can worsen symptoms. Managing stress can promote healing:
- Practice deep breathing or meditation.
- Exercise regularly (walking, yoga, cycling swimming).
- Get enough sleep (7-9 hours per night).
c) Quit Smoking and Limit Alcohol
- Smoking slows down ulcer healing and increases recurrence.
- Alcohol irritates the stomach lining and can make ulcers worse
3. Home Remedies for Peptic Ulcer Disease
While medical treatment is essential for peptic ulcers, some natural remedies may help soothe symptoms and promote healing. These remedies are not a substitute for doctor-prescribed treatments but may provide additional relief:
- Honey
- Honey has natural antibacterial properties and may help fight H. pylori, one of the main causes of ulcers.
- It also helps with wound healing, which may aid in ulcer recovery.
- Aloe Vera Juice
- Aloe vera has anti-inflammatory properties and may help soothe the stomach lining.
- Some studies suggest it can reduce acid production and help with acid reflux symptoms.
- Probiotics (Yogurt, Fermented Foods, Supplements)
- Probiotics introduce good bacteria that help restore balance in the gut.
- Some studies show probiotics may reduce H. pylori levels and improve ulcer healing.
- Cabbage Juice
- Cabbage is rich in vitamin C and has been used as a natural ulcer remedy.
- Some studies suggest it may promote healing by strengthening the stomach lining.
- Turmeric
- Contains curcumin, which has anti-inflammatory and antibacterial effects.
- May help reduce acid secretion and improve gut health.
- Ginger
- Has been traditionally used to aid digestion and reduce nausea.
- Some studies suggest it may help fight H. pylori and reduce stomach irritation.
PLEASE NOTE
- While these remedies may help, they should not replace medical treatment.
- Consult your doctor before trying these remedies, especially if you’re taking ulcer medications or any other medications
- Avoid excessive use
When to See a Doctor
- Seek medical attention immediately if you experience:
- Vomiting blood (bright red or coffee-ground appearance).
- Black, tarry stools (a sign of bleeding).
- Severe stomach pain that doesn’t go away.
- Unexplained weight loss.
These could indicate complications like bleeding, perforation, or obstruction, requiring urgent treatment.
Final Thoughts
- Avoid excessive NSAID use – Take with food and use the lowest effective dose.
- Get tested for H. pylori if you have a history of ulcers.
- Maintain a balanced diet with gut-friendly foods.
- Manage stress through relaxation techniques.
- Quit smoking and reduce alcohol intake.
Peptic ulcers are painful but treatable. With the right combination of medication, lifestyle changes, and dietary adjustments, most ulcers heal within 4 to 8 weeks.
If you suspect you have an ulcer, consult a doctor for a proper diagnosis and treatment plan. Early treatment can prevent serious complications and help you get back to living pain-free.
Additional Resources
H. pylori Testing & Diagnosis – CDC

