I. Introduction
Let’s talk about blood sugar. You’ve probably heard terms like random Blood no sugar or fasting blood sugar, but what do they mean?
Blood sugar, or glucose, is essential because it’s your body’s main source of energy. Every cell in your body needs glucose to function, from your muscles to your brain. But if your blood sugar levels are too high or too low, it can cause serious health problems. Keeping your blood sugar in the normal sugar level range is crucial for staying healthy.
So, how do you know what’s normal and when it’s time to worry? That’s exactly what we’ll cover in this guide
What Are Blood Sugar Levels?
Blood sugar refers to the amount of glucose present in your bloodstream. Your body gets glucose from the food you eat, especially carbohydrates like bread, pasta, and fruits.
Once digested, the glucose enters your bloodstream and travels to your cells.
But here’s where it gets interesting: your body needs insulin to help move that glucose from the blood into the cells where it’s used for energy. The pancreas, a small organ behind the stomach, releases insulin when it detects higher blood sugar levels. If your body doesn’t make enough insulin, or if it can’t use insulin properly, your blood sugar can stay too high—leading to diabetes.
In addition to insulin, the hormone glucagon helps keep blood sugar levels from getting too low. It triggers your liver to release stored glucose into the bloodstream when your levels drop too much.
These two hormones work together to keep your blood sugar balanced and ensure your cells always have the energy they need.
Normal Blood Sugar Ranges
Let’s break down what’s considered normal at different times:
A. Fasting Blood Sugar Normal Range
The fasting blood sugar normal range is what you measure when you haven’t eaten anything for at least 8 hours, typically measured in the morning before breakfast.
This test helps your doctor understand how well your body regulates glucose when it’s not influenced by food.
- A normal fasting blood sugar level is typically between 70 and 99 mg/dL. Anything above 100 mg/dL but below 126 mg/dL is considered prediabetes, which means your blood sugar is higher than normal but not yet high enough to be diagnosed as diabetes.
- A fasting blood sugar level of 126 mg/dL or higher on two separate tests may indicate diabetes.
B. Postprandial (After-Meal) Blood Sugar
This test measures your blood sugar level a couple of hours after eating. Your body digests food, and glucose enters your bloodstream, which causes your blood sugar to rise.
- A normal sugar level two hours after eating is less than 140 mg/dL. If your blood sugar is between 140 mg/dL and 199 mg/dL, this could indicate prediabetes.
- Anything above 200 mg/dL is a potential sign of diabetes.
C. Random Blood Sugar
This test is taken at any time of the day, regardless of when you last ate.
- A normal sugar level range for random blood sugar is under 200 mg/dL.
If it’s higher than this, especially with symptoms of high blood sugar (like increased thirst, fatigue, or frequent urination), your doctor may suggest further testing to rule out diabetes.
D. HbA1c Levels
The HbA1c test measures your average blood sugar level over the past 2-3 months. Unlike the daily or after-meal tests, this test gives a longer-term view of how well your body is managing blood sugar.
- A normal HbA1c level is below 5.7%.
- A result between 5.7% and 6.4% indicates prediabetes, while 6.5% or higher signals diabetes.
Types of Blood Sugar Test
There are two main types of blood sugar tests used to check your blood sugar levels:
1. Capillary Blood Glucose Test
This is the most common test for checking blood sugar. A healthcare professional collects a drop of blood, usually from a fingertip prick. This test involves a test strip and a glucose meter (glucometer), which provide your blood sugar reading within seconds. It’s a quick and convenient way to check your blood sugar levels, especially in a doctor’s office or clinic.
2. Venous (Plasma) Blood Glucose Test
For this test, a phlebotomist collects a sample of blood from a vein (usually in your arm). Venous blood glucose tests are often part of a blood panel, such as a basic metabolic panel, and the samples are sent to a lab for analysis. A medical laboratory scientist processes the sample and runs the test on machines called analyzers. These tests are generally more accurate than capillary blood glucose tests.
At-Home Blood Sugar Testing
For people with diabetes, especially those with Type 1 diabetes, regular blood sugar testing is essential to manage the condition effectively. At-home blood sugar testing is done using a glucometer, which provides quick results. People with diabetes may need to check their blood sugar multiple times a day, depending on their treatment plan.
An alternative to traditional blood glucose testing is the Continuous Glucose Monitoring (CGM) device. These devices provide real-time data on your blood sugar levels throughout the day, helping you track patterns and make adjustments to your treatment plan as needed.
Factors That Affect Blood Sugar Levels
Several things can affect your blood sugar, even if you’re generally healthy:
- Diet
What you eat directly impacts your blood sugar levels. Foods high in simple sugars or refined carbs (like white bread, candy, and sugary drinks) can cause a quick spike in blood sugar. On the other hand, foods that are high in fiber, healthy fats, and proteins can help keep your blood sugar more stable. Eating a balanced diet with plenty of vegetables, whole grains, and lean proteins can help your body manage blood sugar levels more efficiently.
- Physical Activity
Exercise plays a crucial role in managing blood sugar. When you work out, your muscles use glucose for energy, which helps lower your blood sugar. Regular physical activity, especially aerobic exercise like walking, cycling, or swimming, can help your body use insulin more effectively. It’s recommended to get at least 150 minutes of moderate-intensity exercise each week. Skipping workouts, however, can lead to higher blood sugar levels over time, particularly in people with insulin resistance or diabetes.
- Stress and Hormones
Stress can cause your blood sugar to rise. When you’re stressed, your body releases stress hormones like cortisol and adrenaline, which can trigger the liver to release more glucose into the bloodstream. Chronic stress, if left unmanaged, can contribute to higher blood sugar levels over time. It’s essential to find ways to manage stress, whether through relaxation techniques, exercise, or talking to a therapist.
- Medications and Health Conditions
Certain medications can impact your blood sugar levels. For example, steroids, which are often used for inflammation, can raise blood sugar. Some conditions, like polycystic ovary syndrome (PCOS), also make it harder for your body to regulate blood sugar. If you have a health condition or are taking medications that affect your blood sugar, be sure to talk to your doctor about how to manage it.
What Happens When Blood Sugar Levels Are Too High or Too Low?
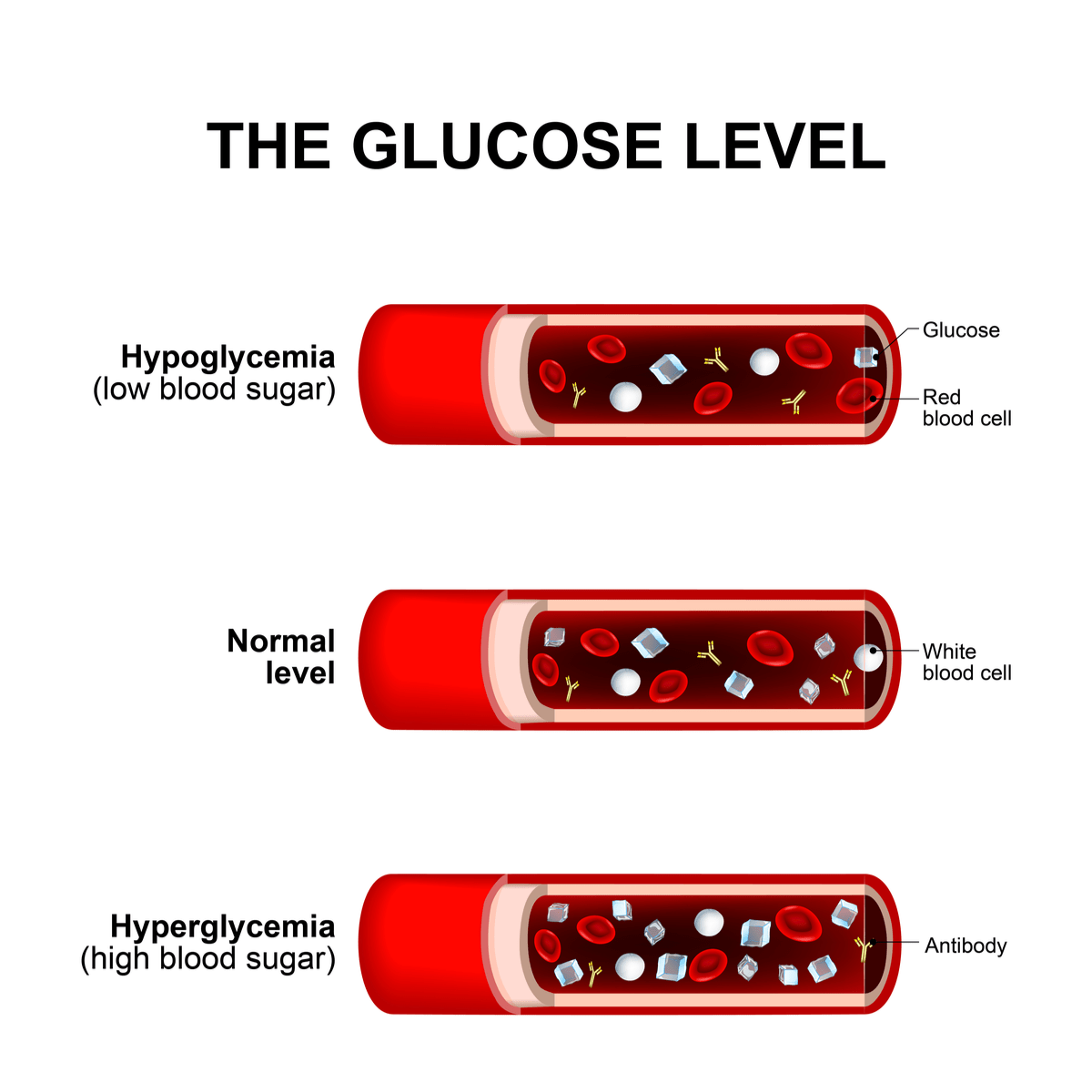
Hyperglycemia refers to blood sugar levels that are too high. A level consistently above 180 mg/dL after meals or 125 mg/dL fasting is a sign that your body is struggling to keep blood sugar under control. Over time, if hyperglycemia is not addressed, it can lead to serious complications.
Symptoms of High Blood Sugar
- Increased thirst
- Frequent urination
- Fatigue or feeling sluggish
- Blurred vision
These are common signs that your blood sugar may be too high.
But when hyperglycemia becomes chronic, it can lead to a range of health problems, including:
- Cardiovascular issues: High blood sugar can damage blood vessels, raising the risk of heart disease and stroke.
- Nerve damage (neuropathy): Excess sugar in the blood can cause nerve damage, leading to pain, numbness, or tingling, especially in the hands and feet.
- Kidney damage: Over time, high blood sugar can harm the kidneys, potentially leading to kidney disease or failure.
If your blood sugar remains consistently high or you notice symptoms like blurry vision, weight loss, or extreme thirst, it’s time to see a doctor.
On the other hand, Hypoglycemia occurs when your blood sugar drops too low, typically below 70 mg/dL. Low blood sugar can be dangerous, especially if you don’t treat it quickly.
Symptoms of Low Blood Sugar
- Shakiness
- Sweating
- Confusion or dizziness
- Hunger or irritability
If you start feeling any of these symptoms, it’s important to check your blood sugar immediately and treat it if necessary.
Severe hypoglycemia can cause serious problems, including:
- Seizures
- Loss of consciousness
- Accidents or injuries due to impaired judgment or coordination
If you have frequent episodes of hypoglycemia or find it difficult to manage, talk to a doctor. Your treatment plan may need to be adjusted.
How to Monitor Your Blood Sugar Levels
- Who Should Monitor?
If you have diabetes, prediabetes, or risk factors like a family history, it’s important to monitor your blood sugar regularly. Even if you don’t have diabetes, it can be useful to keep track if you’re at risk.
- Tools You Can Use
- Glucometer: A small device that measures your blood sugar level with a quick finger prick.
- Continuous Glucose Monitors (CGMs): A wearable device that continuously tracks your blood sugar throughout the day.
- HbA1c Tests: Your doctor can do a blood test every few months to see how well your blood sugar has been controlled over time.
Tips for Accurate Monitoring
To get reliable readings, test your blood sugar at the correct times (such as fasting in the morning or after meals) and follow the instructions provided with your glucometer or continuous glucose monitor.
Testing at the same time each day can help you notice patterns in your blood sugar levels.
It’s also important to keep your testing equipment clean and to replace any used components, like test strips, on time.
When to Worry
While normal fluctuations in blood sugar levels are natural, certain signs can indicate that something is wrong. Be aware of the following red flags that may suggest an issue with your blood sugar:
- Consistently high or low readings: If your blood sugar is frequently outside the normal sugar level range—whether too high or too low—it could signal a problem that needs medical attention.
- Frequent symptoms of hyperglycemia: Increased thirst, frequent urination, fatigue, and blurry vision are all signs that your blood sugar may be too high.
- Symptoms of hypoglycemia: If you experience shakiness, dizziness, or confusion, your blood sugar may be too low. It’s important to address this immediately by eating something with sugar.
- Unexplained weight loss or gain: Significant changes in weight without a clear cause could be a sign of an underlying blood sugar issue, particularly if they are accompanied by other symptoms.
If you experience any of these signs regularly, it’s important to seek medical advice. Early detection and management of blood sugar issues can prevent more serious complications in the future.
Conclusion
Understanding your blood sugar levels is an important part of maintaining good health. Whether it’s fasting blood sugar, random blood sugar, or post-meal readings, knowing what’s considered normal and when to be concerned can help you take control of your health. Regular monitoring, a balanced diet, staying active, and managing stress are all key factors in keeping your blood sugar within a healthy range.
If anything feels off, don’t hesitate to reach out to a healthcare provider. They can help you interpret your blood sugar readings and make any necessary adjustments to your lifestyle or treatment plan.